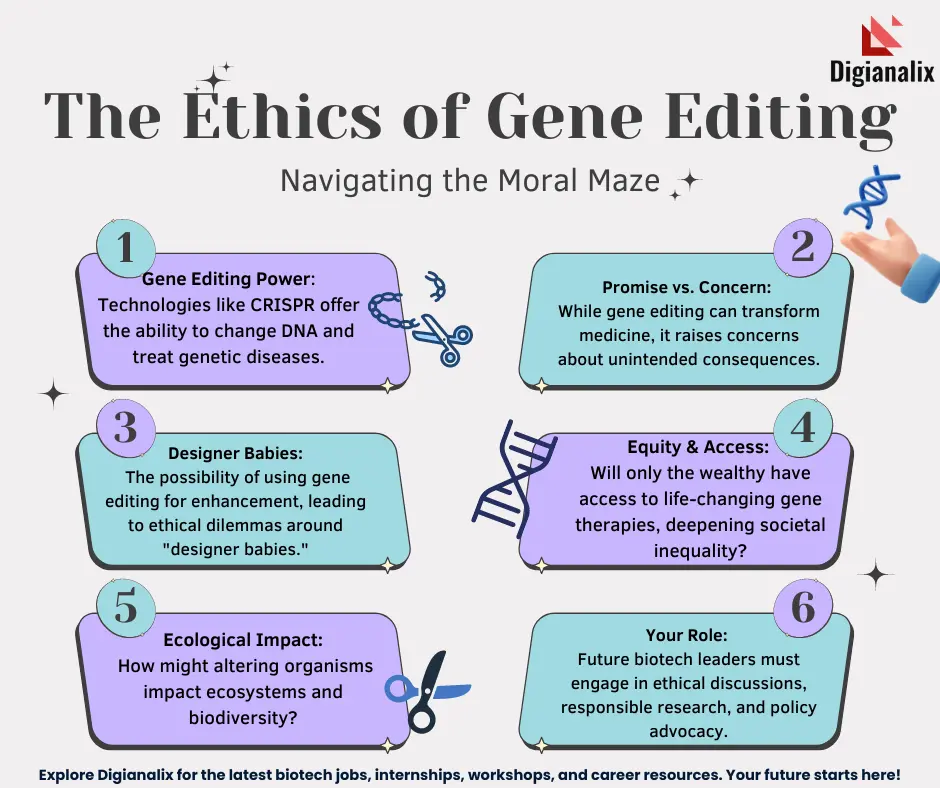
Gene editing ethics is an essential topic in today’s rapidly evolving biotechnological landscape. As advancements in CRISPR technology unveil the potential to cure diseases like sickle cell anemia, profound ethical questions emerge about our right to manipulate the human genome. Balancing the promise of gene manipulation against the risks poses significant challenges, particularly in discussions of health equity and access to these groundbreaking treatments. Engaging in medical ethics discussions surrounding gene editing becomes crucial as we evaluate not just the science, but the societal implications of such powerful tools. Ultimately, striking a balance between innovation and ethical responsibility will shape the future of gene therapy and its accessibility to all.
The ethics of genetic modification and manipulation, especially with groundbreaking techniques like CRISPR, calls for careful consideration. As researchers make strides in developing potential cures for various genetic disorders, such as hemoglobinopathies, we must grapple with the moral implications of our newfound capabilities. This discourse involves evaluating not only the medical efficacy of such interventions but also their accessibility and fairness across different populations. The societal impact of these advancements raises important questions about who benefits from genetic therapies and what constitutes a viable approach to health justice. Thus, discussions around gene editing must encompass broader themes of human rights and equity in health care.
Understanding CRISPR Technology: A Breakthrough in Genetic Medicine
CRISPR technology represents one of the most significant advancements in genetic medicine, enabling precise editing of DNA. Scientists can manipulate both somatic and germline genes, allowing for potential cures for genetic disorders such as sickle cell anemia. This technology’s capacity to accurately clip out and replace specific segments of DNA raises hopes for revolutionary treatments that could transform lives. For instance, by targeting the genetic mutations responsible for sickle cell disease, researchers have successfully demonstrated the ability to reroute the disease’s pathology, paving the way for potential cures.
However, as with any breakthrough, CRISPR also invites a myriad of questions and considerations. While the medical benefits are substantial, the implications of gene editing extend beyond direct health outcomes. There are concerns regarding the long-term effects of such modifications, not only on the individuals treated but also on future generations. The ability to alter germline cells suggests a permanence that could reshape human genetics infinitely. As we delve deeper into this field, understanding the nuances of CRISPR technology becomes critical for both practitioners and patients alike.
Navigating the Ethical Landscape of Gene Editing
The ethical implications of gene editing technologies like CRISPR are profound and complex. During discussions on gene manipulation, a significant concern arises about the morality of altering human traits. For example, when considering whether to use CRISPR to alter embryos in light of conditions like Down syndrome, important ethical questions must be addressed. Who determines which traits are deemed undesirable? This reflects a broader debate in medical ethics discussions regarding the acceptable boundaries of human enhancement versus necessary medical intervention.
Moreover, the ethical framework surrounding gene editing is intertwined with health equity issues. As highlighted in discussions about the cure for sickle cell anemia, the high cost of treatment poses challenges to access, potentially exacerbating existing health disparities. The need for a comprehensive view that encompasses both the science and its ethical ramifications is essential to navigate these potentially murky waters. Establishing guidelines and ethical standards will be crucial in ensuring that advancements in gene editing serve humanity broadly rather than amplifying inequities.
Economic Implications of Gene Therapies: Who Can Afford Them?
The economic implications of new gene therapies, such as the estimated $2.2 million cost for sickle cell anemia treatment, reveal deep systemic challenges in healthcare access. The price tag raises an important issue of distribution: who has the financial resources to afford such life-saving interventions? The disparity points to a troubling reality where innovation could widen the gap between those with means and those without, ultimately questioning the fairness of medical progress. This also highlights the necessity for policies that can address these financial barriers and ensure equitable access to revolutionary treatments.
Furthermore, the financial burden of gene editing technologies can lead to significant debates about healthcare equity. As some patients experience the life-changing benefits of CRISPR, many others may be left behind due to economic constraints. This disparity poses a question of social responsibility; as the medical community advances in gene editing, there must also be intentional efforts to create inclusive policies that serve all populations. The long-term success of these technologies will depend not only on their scientific efficacy but also on their accessibility to varied demographics.
Potential Unintended Consequences of Gene Editing
As we harness the power of CRISPR technology, the potential for unintended consequences cannot be overlooked. Manipulations at the genetic level could yield unforeseen effects that may not be immediately apparent, raising questions about safety and long-term outcomes. For instance, editing the gene controlling LDL cholesterol may lower ‘bad’ cholesterol levels but could disrupt other biological functions essential for health. This complexity of genetic interactions reminds us that our understanding of the human genome, while expanding, is still far from complete.
The unpredictable nature of gene editing highlights the importance of thorough oversight and ethical considerations. As noted in discussions around germline editing, the potential for creating changes that could be passed down through generations underscores the urgency for robust regulatory frameworks. Ensuring these technologies are utilized safely and responsibly will necessitate a concerted effort by scientists, ethicists, and policymakers alike to mitigate risks while maximizing benefits.
CRISPR and Health Equity: Balancing Benefits and Access
The discussion of CRISPR technology cannot be separated from its implications for health equity. As this powerful tool enables the potential cure for diseases like sickle cell anemia, it also raises critical questions about access to such treatments. Without equitable distribution of these innovations, we risk creating a system where only the wealthy can afford to benefit from groundbreaking medical advancements, thereby perpetuating existing health disparities. Efforts must be made to integrate health justice considerations into the development and implementation of gene editing therapies.
To foster true equity in healthcare, it is vital that policymakers and healthcare leaders work together to develop strategies that ensure all populations have access to innovative treatments, regardless of socioeconomic status. Addressing these disparities is not just an ethical obligation but a moral imperative that challenges us to create a fairer healthcare system for future generations. By placing health equity at the forefront of gene editing discussions, we move closer to a future where medical advancements benefit everyone, rather than a select few.
The Intersection of Medical Ethics and Gene Manipulation
Medical ethics discussions are paramount when considering the application of gene manipulation technologies. The profound implications of editing human genes compel us to reflect on the moral responsibilities that accompany such power. Ethical questions about consent, especially in germline editing where the decisions impact future generations, are vital to the discourse. As we navigate the landscape of gene editing, it is imperative that ethical considerations remain intertwined with scientific advancements to ensure responsible use.
Furthermore, considering the implications of gene editing on the concept of human variation adds another layer to this ethical framework. As some advocate for the modification of traits to eliminate perceived pathologies, the risk of devaluing natural diversity can lead to societal pressures to conform to narrow standards of health and ability. Addressing these concerns in medical ethics discussions will help shape a more inclusive and thoughtful approach to gene manipulation that respects human differences while advancing science.
A Historical Perspective on Medical Innovations and Ethics
Historically, significant medical innovations have often been accompanied by ethical dilemmas. From the introduction of anesthesia to the use of antibiotics, advancements have continually challenged our moral compass. As we look to the future with gene editing technologies like CRISPR, it is crucial to draw lessons from past experiences in medicine. Reflecting on historical case studies provides insight into how society has grappled with the ethical ramifications of new treatments, offering valuable perspectives on navigating today’s challenges.
Understanding the historical context of medical ethics allows us to appreciate the evolving conversation around healthcare practices. With every significant breakthrough, there has been a need for regulatory frameworks and ethical guidelines to protect patients and ensure that innovations serve the greater good. As we embrace the promise of gene editing, it is essential to remain vigilant, learning from history to foster a responsible approach that prioritizes patient welfare and societal values.
Public Perception and the Future of Gene Editing
Public perception plays a critical role in the future of gene editing technologies. As advancements in CRISPR become more widespread, the general public’s understanding and acceptance of these innovations significantly influence policy and regulation. Misinformation and lack of awareness can breed fear and skepticism, which may hinder progress and implementation. Therefore, fostering transparent dialogues around the benefits, risks, and ethical concerns of gene editing is essential for constructing a well-informed populace that can engage with these critical issues.
Additionally, as audiences become more engaged in discussions regarding gene editing, there is an opportunity to advocate for a balanced narrative that emphasizes both the potential and the ethical considerations. By incorporating public input into the decision-making process surrounding gene technology, we foster a collaborative approach that reflects societal values and priorities. Ensuring that diverse voices are included in these discussions will pave the way for more equitable outcomes in the realm of medical innovation.
The Role of Regulatory Frameworks in Gene Editing
The establishment of robust regulatory frameworks is fundamental to the successful and ethical application of gene editing technologies. As innovations like CRISPR advance, regulatory bodies face the challenge of creating policies that ensure scientific exploration and patient safety. Effective regulations will not only address the safety and efficacy of new treatments but also consider their social and ethical implications, ensuring that progress does not outpace ethical considerations.
Regulation must also adapt to the rapid changes in genetic science, keeping pace with emerging technologies while remaining flexible enough to address unforeseen challenges. Collaboration between scientists, ethicists, and policymakers is vital in developing comprehensive guidelines that govern the use of gene editing and protect vulnerable populations from potential misapplications. As we move forward, the commitment to effective regulation will be crucial in shaping the responsible use of gene editing technologies.
Frequently Asked Questions
What are the ethical implications of using CRISPR technology in gene editing?
The ethical implications of using CRISPR technology in gene editing revolve around issues such as consent, the potential for unintended consequences, and the societal impacts of genetic modifications. Discussions center on whether it is morally acceptable to edit human genes, especially in germline cells, which affect future generations. There are concerns about who has the right to make decisions regarding genetic alterations, particularly for diseases that are not life-threatening. The need for responsible oversight in gene editing practices is crucial to address these ethical concerns.
How might gene editing impact health equity among different populations?
Gene editing, particularly through CRISPR technology, raises significant questions about health equity. The high costs associated with treatments, like the sickle cell anemia cure which can reach around $2.2 million, create disparities in access to these innovations. Marginalized populations may not afford these gene therapies, exacerbating existing healthcare inequalities. Discussions in medical ethics emphasize the need for equitable distribution and access to gene editing technologies to ensure that all individuals can benefit from advancements, regardless of socioeconomic status.
What are the risks of gene manipulation in CRISPR applications?
The risks of gene manipulation in CRISPR applications include unintended genetic mutations, off-target effects, and long-term health consequences that may not be immediately apparent. These risks underscore the complexity of the human genome, as genes interact with each other and with various biological systems. Ethical discussions in the field highlight the importance of thorough research and monitoring to mitigate these risks before widespread clinical application of gene editing techniques.
Should gene editing be used to alter traits compatible with life, such as in individuals with Down syndrome?
The ethical debate surrounding gene editing for traits compatible with life, like Down syndrome, is contentious. Some argue that such modifications could enhance quality of life, while others believe it undermines the value of diversity and raises concerns about parental rights over their child’s genetic makeup. Medical ethics discussions emphasize the need for societal dialogue and ethical frameworks to guide decisions about what constitutes acceptable uses of gene editing technology.
What role does oversight play in ensuring responsible gene editing practices?
Oversight is critical in ensuring responsible gene editing practices, especially with technologies like CRISPR that have profound implications for human genetics. Effective regulatory frameworks must be established to monitor research and applications, preventing misuse, such as unregulated gene editing for enhancement purposes. Moreover, ethical oversight can help address concerns related to consent, equity, and the potential for creating a divide between those who can afford gene editing and those who cannot.
How does CRISPR technology challenge traditional medical ethics discussions?
CRISPR technology challenges traditional medical ethics discussions by introducing new dilemmas regarding the morality of altering human genetics. It prompts questions about the definition of treatment versus enhancement, and the ethical implications of creating genetically modified organisms, including humans. With the power to manipulate genes comes responsibility, necessitating a reevaluation of existing ethical frameworks to accommodate the rapid advancements in gene editing technologies and their societal impacts.
| Key Points | Details | |
|---|---|---|
| Ethical Dilemmas of Gene Editing | The central question is whether we should use gene editing to change human traits, such as in sickle cell disease treatment. | |
| Challenges of CRISPR Technology | CRISPR allows editing both somatic and germline genes, raising questions about long-term consequences and ethical implications. | |
| Cost and Accessibility | The high cost of gene editing treatments, such as the sickle cell cure costing $2.2 million, highlights health equity issues. | |
| Health Justice | Innovation in gene editing often benefits those who already have resources, widening the gap in health justice. | |
| Parental Decisions on Genetic Traits | Questions persist about the right of parents to choose genetic traits for their children and the societal implications of such choices. | |
| Unintended Consequences | Gene editing might have unforeseen effects due to the complex interactions of genes, as seen with changes to cholesterol-related genes. | |
Summary
Gene editing ethics refers to the moral implications of altering the human genome, as highlighted in the discussion of CRISPR technology’s potential and pitfalls. As researchers and practitioners explore the efficacy of gene editing in curing diseases, we must grapple with fundamental ethical questions about altering human traits and behaviors. Addressing issues of health equity and parental responsibility will be essential as advances continue in this field, ensuring that progress does not come at the expense of ethical considerations.